Which Are The Primary Reasons For Over-Pronation
Over Pronation (Flat Feet) refers to the biomechanical shock-absorbing motion of the ankle, foot and lower leg. It is the natural inward flexing motion of the lower leg and ankle. Standing, walking, and running cause the ankle joint to pronate which in turn helps the body to absorb shock and allows it to control balance. An ankle joint that is too flexible causes more pronation than desired. This common condition is called Over- Pronation (sometimes referred to as "Flat Feet"). This foot condition places an extreme degree of strain on various connective tissues of the ankle, foot, and knee. If this condition is not addressed foot pain and toe deformities such as bunions and hammer toes (just to name a couple) may develop. Hip and lower back pain may also be residual results from this condition.

Causes
There are many biomechanical issues that can contribute to excessive pronation, including weak foot intrinsic muscles, limited ankle dorsiflexion mobility and calf flexibility, weak ankle invertor muscles (e.g. posterior tibialis), weak forefoot evertor muscles (peroneus longus), poor hip strength and control, Anterior pelvic tilting, heel InversionIn a person who overpronates, the heel bone goes into an everted position meaning that it turns out away from the midline of the body. The opposite motion of eversion is inversion. Inversion is a motion that needs to be controlled to prevent the foot from excessively pronating.
Symptoms
Because overpronation affects the entire lower leg, many injuries and conditions may develop and eventually cause problems not only in the leg and foot, but also the knee, hips and lower back. Pain often begins in the arch of the foot or the ankle. Blisters may develop on the instep, or on the inside edge of the heels. As overpronation continues and problems develop, pain will be felt elsewhere, depending on the injury.
Diagnosis
The best way to discover whether you have a normal gait, or if you overpronate, is to visit a specialty run shop, an exercise physiologist, a podiatrist or a physical therapist who specializes in working with athletes. A professional can analyze your gait, by watching you either walk or run, preferably on a treadmill. Some facilities can videotape your gait, then analyze the movement of your feet in slow-motion. Another (and less costly) way is to look at the bottom of an older pair of run shoes. Check the wear pattern. A person with a normal gait will generally see wear evenly across the heel and front of the shoe. A person who overpronates will likely see more wear on the OUTside of the heel and more wear on the INside of the forefoot (at the ball). A person who supinates will see wear all along the outer edges of the shoe. You can also learn about your gait by looking at your arches. Look at the shape your wet feet leave on a piece of paper or a flat walking surface.
Non Surgical Treatment
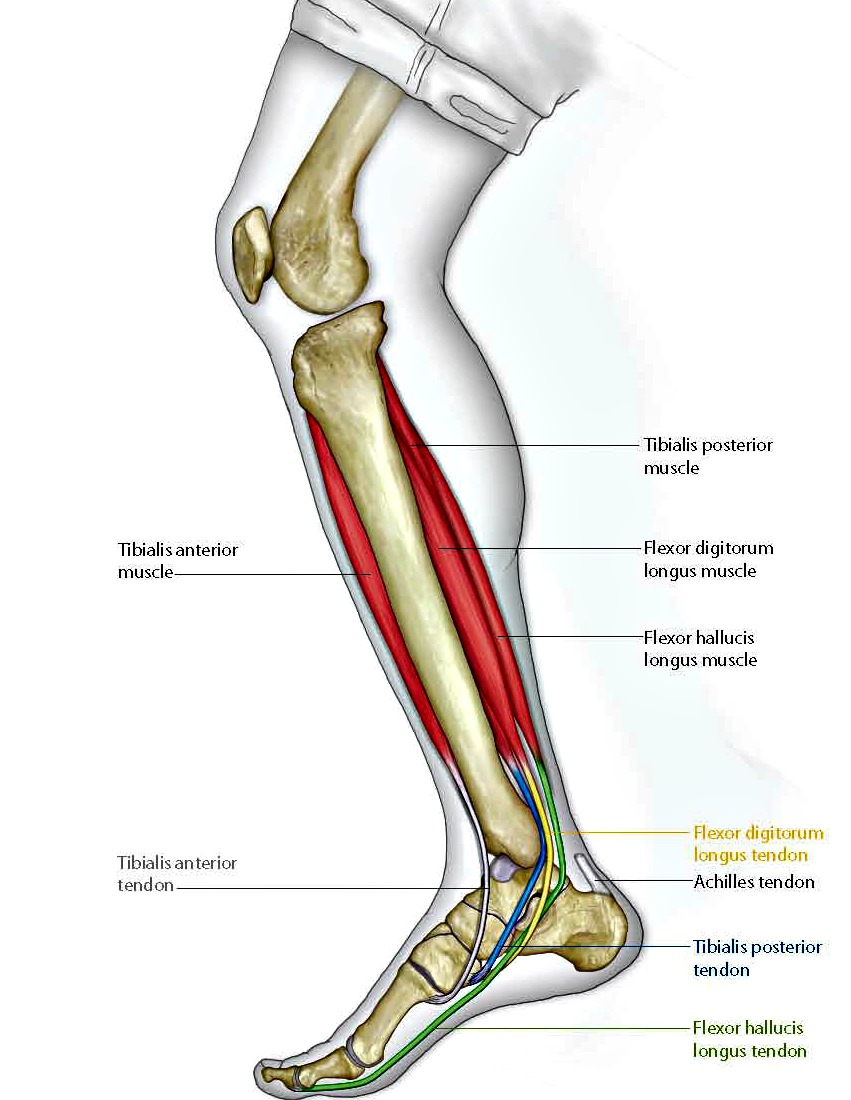
The following exercises help retrain the foot and ankle complex to correct overpronation. Exercises may be performed while wearing shoes, or for an even greater challenge, in bare feet. Duck Stand. This exercise is designed to prepare for the more dynamic BT exercises ahead by waking up the gluteal muscles and teaching clients how the gluteal muscles control the degree of foot pronation. For example, when the glutes contract concentrically, they rotate the leg outward. As the leg rotates outward, the arch of the foot raises (i.e., supinates). Stand beside the BT with both heels together and feet turned outward. (Note: As you progress, perform this exercise while standing on the BT.) Try to rotate legs outward by tightening buttock muscles while tilting pelvis under. As legs rotate outward, arches of the feet raise up out of pronation. Hold position for 30 seconds. Big Toe Pushdowns. This exercise is designed to strengthen the muscle of the big toe that holds up the arch of the foot (i.e., flexor hallucis longus muscle). This stops the foot from overpronating. Stand on top of the BT dome with feet facing forward. Use gluteal muscles to raise the arches of the feet (see previous exercise - "Duck Stand"). Keep arches raised while pushing down big toe into the BT. While pushing down, tension build in the arch on the underside of their foot should be felt. Hold position for 15 seconds.
Surgical Treatment
Calcaneal "Slide" (Sliding Calcaneal Osteotomy) A wedge is cut into the heel bone (calcaneus) and a fixation device (screws, plate) is used to hold the bone in its new position. This is an aggressive option with a prolonged period of non-weightbearing, long recovery times and many potential complications. However, it can and has provided for successful patient outcomes.
Addressing Severs Disease
If your child is experiencing activity related pain just below the kneecap, at the top of the shinbone, or in their heel or hip then the chances are they are suffering from Osgood Schlatter, Severs disease or Ischial Apophysitis respectively. Today, thousands of children are diagnosed with one of these conditions every year. Many others are never diagnosed and the discomfort is often dismissed as 'growing pains'
Causes
Sever?s Disease is thought to be caused by several reasons. Growth spurts. The muscles and tendons become tight due to rapid bone growth. Overuse. Sever?s Disease can also occur in children who are athletically active and overwork his or her muscles. Some physicians are beginning to caution parents about checking their children?s shoes to make sure they fit well and do not pinch or put undue pressure on the child?s feet. Pronation can also bring on Sever?s Disease.
Symptoms
Sharp pain will be present in the affected heel (or both heels), especially while running or walking. Pain can be heightened following activity. The area will be tender to the touch and usually becomes inflamed or reddened. It may also be painful to press on the heel with a finger from the back or to squeeze the sides together; the latter is particularly common. You might notice stiffness in some of the surrounding muscles, making regular movements more difficult to achieve. This and the pain can manifest physically in abnormal practices like tiptoeing or limping. In some cases a lump can be detected on the back of the heel, though it may be so small as to defy detection.
Diagnosis
Sever condition is diagnosed by detecting the characteristic symptoms and signs above in the older children, particularly boys between 8 and 15 years of age. Sometimes X-ray testing can be helpful as it can occasionally demonstrate irregularity of the calcaneus bone at the point where the Achilles tendon attaches.
Non Surgical Treatment
First, your child should cut down or stop any activity that causes heel pain. Apply ice to the injured heel for 25 minutes three times a day. Your child should not go barefoot. If your child has severe heel pain, ibuprofen (Advil) will help. It is important that your child performs exercises to stretch the hamstring and calf muscles, and the tendons on the back of the leg. The child should do these stretches five times each, two or three times a day. Each stretch should be held for 20 seconds. Your child also needs to do exercises to strengthen the muscles on the front of the shin. To do this, have your child stand facing a wall to stretch the calves and the heel cord. Place one foot a shoulder?s width in front of the other, both feet facing the wall. The front knee is bent and the back knee is straight during the calf stretch. Then have your child push against the wall and feel the stretch in his or her back leg. To stretch out the heel cord, have him or her stay in the same position and bend the back knee. Repeat three times. Practice this stretch twice daily.
Surgical Treatment
The surgeon may select one or more of the following options to treat calcaneal apophysitis. Reduce activity. The child needs to reduce or stop any activity that causes pain. Support the heel. Temporary shoe inserts or custom orthotic devices may provide support for the heel. Medications. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, help reduce the pain and inflammation. Physical therapy. Stretching or physical therapy modalities are sometimes used to promote healing of the inflamed issue. Immobilization. In some severe cases of pediatric heel pain, a cast may be used to promote healing while keeping the foot and ankle totally immobile. Often heel pain in children returns after it has been treated because the heel bone is still growing. Recurrence of heel pain may be a sign of calcaneal apophysitis, or it may indicate a different problem. If your child has a repeat bout of heel pain, be sure to make an appointment with your foot and ankle surgeon.
What Causes Pain In Arch Of Foot After Running?
Arch pain(medically known as plantar pain)is a broad term many people use to describe pain in their muscles, tendons, ligaments, bones, or nerves. All these components are connected to the bottom of the foot; therefore, damage to any one of these can cause pain on the bottom of the foot. This pain may only last for short time, but can progressively worsen if untreated. Most people who suffer from this pain are between the ages of 30 and 80, but many younger athletes are also susceptible, particularly those who participate in high-impact sports.
Causes
Poor quality footwear. Excess weight. Commonly occurs in people over 50. Overuse or strain by athletes, especially runners. Plantar fasciitis can be caused by overuse of the plantar fascia due to walking or running in poorly supported footwear. It?s not surprising to note that healthy, active adults are the most common victims of plantar fasciitis: runners, joggers, basketball players, tennis and racquetball players? basically any sport that requires quick or repetitive movements combined with impact on the heel and arch of the foot can lead to plantar fasciitis. Seniors are also at risk due to the ligament and bone issues common to those of older years. Another leading cause of plantar fasciitis is being overweight or obese. In this case, while a sports-related injury may not be to blame, just the daily stress of walking with too much excess weight straining the plantar fascia ligaments can lead to inflammation and painful heel pain. Anyone whose job requires long periods of standing or walking is prone to develop plantar fasciitis as well. For those who develop arch strain or arch pain as a result of structural problems like flat feet, they require arch support that will accommodate their individual needs.
Symptoms
Flat feet can exhibit a variety of symptoms, from mild to severe. The extent of the flat foto does not always correlate with the extent of symptoms. Patients may complain of arch pain and heel pain. Commonly there is pain on the outside of the foot, where the foot meets the ankle as the collapse foot abuts against the ankle. Muscle cramps within the foot, and onto the leg (shin splints) may occur. In general, patients have pain with activity, such as walking or running. The pain may be deep and focal to a generalized widespread achy feeling. Irritation from shoe gear can cause redness and swelling. Common reasons patients seek treatment are pain, interference with walking or activities, difficulty fitting shoes, swelling, and notice a change in appearance of the foot and/or unsightly appearance.
Diagnosis
The medical practitioner will examine how the muscles of your foot function. These tests may involve holding or moving your foot and ankle against resistance; you may also asked to stand, walk, or even run. Pain caused by movements may indicate the cause of the pain. The nerves in the foot will be tested to make sure no injury has occurred there. An x-ray, MRI, or bone scan of the foot and arch may be taken to determine if there are changes in the makeup of the bone.
Non Surgical Treatment
An orthotic arch support, specially molded to fit your foot, may be part of your treatment. These supports can be particularly helpful if you have flat feet or high arches. You can tell if that is what is needed when short-term taping decreases your heel pain.

Surgical Treatment
Cavus foot is caused in part by an over-pull of one of the lateral ankle muscles. A release of this tendon can be performed on the outside of the ankle. Additionally, a transfer of this tendon can be performed to help in correcting deformity of the ankle joint. Often patients will have a tightness of their gastrocnemius muscle, one of the main muscles in the calf. This can increase the deformity or prevent a correction from working. It is addressed with a lengthening of a part of the calf muscle or Achilles tendon. This is often performed through one or more small cuts in the back of the leg or ankle. Finally, the plantar fascia may be tight. The plantar fascia is a cord-like structure that runs from the heel to the front part of the foot. Partial or complete plantar fascia release may be done.
Prevention
It is possible to prevent arch pain by wearing well-fitting shoes while performing any physical activity. Many times doctors will suggest a therapeutic shoe with a higher heel to relieve the pressure on the achilles tendon and also the arch muscle (plantar fasciitis). People with arch pain suffer from regular flare-ups of pain. However there is no risk to others as this is not a contagious condition.
Stretching Exercises
Massage therapy is a great way to loosen muscles and help improve mobility in in your feet. As many people with foot pain have discovered, tight muscles in your legs or back can lead to tense foot muscles. All those muscles are connected, so tension in your back can cause tension in your legs which can pull the tendons in your feet and cause stiffness and pain. Getting acupuncture or a professional full body massage are probably the best ways to deal with this, but there are also some simple tricks you can do at home to help keep muscles limber. These are great for loosening up and improving circulation, both before and after exercise. Place a tennis ball under the arch of your bare foot and roll it around, stretching the muscles in your foot and promoting blood flow. You can also roll the ball under your calves and upper legs to work out stiffness and knots. If you feel the tennis ball is too easy, try a lacrosse ball for deeper massaging. This is also demonstrated in the exercise video above. Use a foam roller, those big overpriced rolls of foam that are now available in every department and sporting goods store are fantastic for self-massage (why a roll of foam costs $30 is beyond us, but they do work wonders-our advice is to not waste money on the more expensive fancy grooved ones because even the simplest rollers work great). The exercises you can do with foam rollers seem to be endless, and there are literally hundreds of free videos online showing how to use them to massage every part of your body. Here's one we picked out that specifically targets foot and leg muscles related to arches and plantar fasciitis.
Posterior Tibial Tendon Insufficiency Disorder
Overview
Adult acquired flatfoot deformity (AAFD or AAF) is a progressive, symptomatic deformity resulting from gradual stretch of the posterior tibial tendon as well as other ligaments supporting the arch of the foot. AAFD develops after skeletal maturity, May also be referred to as posterior tibial tendon dysfunction (PTTD), although due to the complexity of the disorder AAFD is more appropriate. Significant ligamentous rupture occurs as the deformity progresses. Involved ligaments include the spring ligament, the superficial deltoid ligament, the plantar fascia, and the long and short plantar ligaments. Unilateral AAFD is more common than bilateral AAFD. 
Causes
Causes of an adult acquired flatfoot may include Neuropathic foot (Charcot foot) secondary to Diabetes mellitus, Leprosy, Profound peripheral neuritis of any cause. Degenerative changes in the ankle, talonavicular or tarsometatarsal joints, or both, secondary to Inflammatory arthropathy, Osteoarthropathy, Fractures, Acquired flatfoot resulting from loss of the supporting structures of the medial longitudinal arch. Dysfunction of the tibialis posterior tendon Tear of the spring (calcaneoanvicular) ligament (rare). Tibialis anterior rupture (rare). Painful flatfoot can have other causes, such as tarsal coalition, but as such a patient will not present with a change in the shape of the foot these are not included here.
Symptoms
Your feet tire easily or become painful with prolonged standing. It's difficult to move your heel or midfoot around, or to stand on your toes. Your foot aches, particularly in the heel or arch area, with swelling along the inner side. Pain in your feet reduces your ability to participate in sports. You've been diagnosed with rheumatoid arthritis; about half of all people with rheumatoid arthritis will develop a progressive flatfoot deformity.
Diagnosis
Although you can do the "wet test" at home, a thorough examination by a doctor will be needed to identify why the flatfoot developed. Possible causes include a congenital abnormality, a bone fracture or dislocation, a torn or stretched tendon, arthritis or neurologic weakness. For example, an inability to rise up on your toes while standing on the affected foot may indicate damage to the posterior tibial tendon (PTT), which supports the heel and forms the arch. If "too many toes" show on the outside of your foot when the doctor views you from the rear, your shinbone (tibia) may be sliding off the anklebone (talus), another indicator of damage to the PTT. Be sure to wear your regular shoes to the examination. An irregular wear pattern on the bottom of the shoe is another indicator of acquired adult flatfoot. Your physician may request X-rays to see how the bones of your feet are aligned. Muscle and tendon strength are tested by asking you to move the foot while the doctor holds it.
Non surgical Treatment
The adult acquired flatfoot is best treated early. Accurate assessment by your doctor will determine which treatment is suitable for you. Reduce your level of activity and follow the RICE regime. R - rest as often as you are able. Refrain from activity that will worsen your condition, such as sports and walking. I - ice, apply to the affected area, ensure you protect the area from frostbite by applying a towel over the foot before using the ice pack. C - compression, a Tubigrip or elasticated support bandage may be applied to relieve symptoms and ease pain and discomfort. E - elevate the affected foot to reduce painful swelling. You will be prescribed pain relief in the form of non-steroidal antiinflammatory medications (if you do not suffer with allergies or are asthmatic). Immobilisation of your affected foot - this will involve you having a below the knee cast for four to eight weeks. In certain circumstances it is possible for you to have a removable boot instead of a cast. A member of the foot and ankle team will advise as to whether this option is suitable for you. Footwear is important - it is advisable to wear flat sturdy lace-up shoes, for example, trainers or boots. This will not only support your foot, but will also accommodate orthoses (shoe inserts). 
Surgical Treatment
If conservative treatments don?t work, your doctor may recommend surgery. Several procedures can be used to treat posterior tibial tendon dysfunction; often more than one procedure is performed at the same time. Your doctor will recommend a specific course of treatment based on your individual case. Surgical options include. Tenosynovectomy. In this procedure, the surgeon will clean away (debride) and remove (excise) any inflamed tissue surrounding the tendon. Osteotomy. This procedure changes the alignment of the heel bone (calcaneus). The surgeon may sometimes have to remove a portion of the bone. Tendon transfer: This procedure uses some fibers from another tendon (the flexor digitorum longus, which helps bend the toes) to repair the damaged posterior tibial tendon. Lateral column lengthening, In this procedure, the surgeon places a small wedge-shaped piece of bone into the outside of the calcaneus. This helps realign the bones and recreates the arch. Arthrodesis. This procedure welds (fuses) one or more bones together, eliminating movement in the joint. This stabilizes the hindfoot and prevents the condition from progressing further.
What Leads To Achilles Tendinitis Problems ?
 Achilles tendinitis (or Achilles tendonitis) is a strain of the Achilles tendon, which connects the calf muscles to the heel bone. Pain can be moderate or severe, but the condition is not usually serious. Of course, if you are suffering the leg and heel pain it brings, it certainly feels serious enough.
Achilles tendinitis (or Achilles tendonitis) is a strain of the Achilles tendon, which connects the calf muscles to the heel bone. Pain can be moderate or severe, but the condition is not usually serious. Of course, if you are suffering the leg and heel pain it brings, it certainly feels serious enough.
Causes
Like any muscle or tendon in the body, the older we get, the more likely we are to sustain an injury. So middle-aged men and women are most at risk, with a slightly higher risk factor attributed to males. Those who participate in more intense athletic activities like high impact sports (tennis, running, basketball) are most susceptible to the injury. Certain underlying medical conditions can also be a contributing factor. Diabetics are more at risk of suffering from Achilles Tendinitis, as are those who are not in great physical shape. Some antibiotics, particularly fluoroquinolones can make one more likely to suffer a strained Achilles Tendon.
Symptoms
Symptoms of Achilles Tendinitis include the following. Pain and stiffness along the Achilles tendon in the morning. Pain along the tendon or back of the heel that worsens with activity. Severe pain the day after exercising. Thickening of the tendon. Bone spur (insertional tendinitis). Swelling that is present all the time and gets worse throughout the day with activity. If you have an Achilles tendon rupture, you might feel a pop or snap, accompanied by a sharp pain behind your ankle. You are likely to have difficulty walking properly. If you have ruptured your Achilles tendon then surgery is likely to be the best treatment option.
Diagnosis
The doctor will perform a physical exam. The doctor will look for tenderness along the tendon and pain in the area of the tendon when you stand on your toes. X-rays can help diagnose bone problems. An MRI scan may be done if your doctor is thinking about surgery or is worried about the tear in the Achilles tendon.
Nonsurgical Treatment
Make sure that the tendon is not torn through and through. If it is severed, you must see a doctor immediately so that the tendon can be repaired. Severe injuries can sever a tendon, without a skin laceration being present. Testing involves moving the toes and foot to see if the tendon moves. If the tendon does not appear to move, it may be severed (comparing the injured tendon and its movement to the same tendon on the uninjured foot may help). Very sharp pain, a sudden pop, or an obvious gap in the structure of the tendon are all signs of a rupture, and should be seen by a doctor as soon as possible. If there is extreme swelling of the leg, and pain (out of proportion to the amount of trauma received), you may have sustained a vascular injury. A doctor must see this type of injury immediately. If you are not sure, see a doctor. If you have multiple injured areas see a doctor immediately, in order to prevent excessive swelling and pain. If the above exam is negative, then you may proceed with self-treatment. (However, if you are not sure of the extent of your injury, you should consult your doctor immediately). The sooner you begin to treat your injury by following "R.I.C.E.", the better you will feel. Rest is very important. Take off your shoe, get off your feet, and relax. Ice should be applied as soon as possible. Never apply ice directly on the injured area, as the cold may make the pain worse. Ice should be applied close to the injured site, between the heart and the injury, so that as the blood flows under the ice, it will be cooled. This cool blood flowing into the injured area will help to reduce the swelling and pain. Apply the ice, wrapped in a cloth or over an elastic bandage, to the foot for 15 minutes, every 1-2 hours, for up to 3 days after an injury. If the ice is uncomfortable, or causes increased pain, do not continue to use it, and see a doctor. If you have poor circulation do not use ice, as this may cause a serious problem. c. Compression is used to limit swelling, and to give support to the injured area. Compression should be applied to the entire foot, starting first at the toes and working back to the ankle. If it is applied just to the injured area, increased swelling will occur in front and behind the wrapping. Compression should be applied with a 3-inch elastic bandage, beginning around the base of all the toes, and then going around the foot and ankle. Continue over the calf muscle when possible. Compression reduces motion in the injured area and foot, and this decreases the pain, and allows for quicker healing. The bandage should not be so tight that it causes increased pain or throbbing in the toes or foot. It should be comfortable! Do not remove the elastic bandage for the first 12 hours, unless it becomes too tight, or the pain increases, or the toes become pale, blue, or cool. If any of these things happen, immediately remove all bandages, and leave them off for several hours. The normal color and temperature of the toes should return immediately. If not, see a doctor immediately! Continue until the swelling and pain subsides; it could take from several days to several weeks. d. Elevation of the leg will aid in reducing swelling and pain. Blood rushes to an injured area to bring increased blood cells, that aid in healing. Gravity will also force blood to the injured area. Too many cells and too much fluid will apply pressure to the injured nerves and tissues, and cause increased pain and delayed healing. Keep your foot elevated so that it is at least parallel to the ground, or higher if it is comfortable. Do this for at least 48 hours, or until the throbbing subsides, when you lower the leg.

Surgical Treatment
Surgery usually isn't needed to treat Achilles tendinopathy. But in rare cases, someone might consider surgery when rubbing between the tendon and the tissue covering the tendon (tendon sheath) causes the sheath to become thick and fibrous. Surgery can be done to remove the fibrous tissue and repair any small tendon tears. This may also help prevent an Achilles tendon rupture.
Prevention
Maintaining strength and flexibility in the muscles of the calf will help reduce the risk of tendinitis. Overusing a weak or tight Achilles tendon makes you more likely to develop tendinitis.
Pes Planus What You Should Expect

It is rare to find someone who walks with both feet in perfect alignment. A foot that is flat or has a very high arch does not necessarily require treatment unless there is pain. Often we walk on the inside or outsides of our feet, or with our toes or heels rotated inward or outward more than they should be. These atypical walking patterns can cause many problems not just with the feet but also for the whole body as the alignment of the feet sets the foundation for the whole body?s alignment. One of the most common effects of improper alignment is known as flatfoot, or pes planus.
Causes
Fallen arches can be the result of other conditions such as overuse, stretching or tearing of the posterior tibial tendon (which attaches to a bone in the foot and runs up the calf of the lower leg at a tension which pulls up the arch) which reduces its ability to maintain tension in the tendon. Whether or not the condition is caused by overpronation, this is the likely outcome for runners, whose arches are no longer strong enough to take the constant strain of bearing the body?s weight on impact, causing joint, postural and muscular problems.
Symptoms
Symptoms that should be checked by a pediatrician include foot pain, sores or pressure areas on the inner side of the foot, a stiff foot, limited side-to-side foot motion, or limited up-and-down ankle motion. For further treatment you should see a pediatric orthopedic surgeon or podiatrist experienced in childhood foot conditions.
Diagnosis
Flat feet are easy to identify while standing or walking. When someone with flat feet stands, their inner foot or arch flattens and their foot may roll over to the inner side. This is known as overpronation. To see whether your foot overpronates, stand on tiptoes or push your big toe back as far as possible. If the arch of your foot doesn't appear, your foot is likely to overpronate when you walk or run. It can be difficult to tell whether a child has flat feet because their arches may not fully develop until they're 10 years of age.
Non Surgical Treatment
If you have flat feet, you may also experience pain throughout the lower body and into the lower back. Orthotics (custom-made rigid foot supports) can be prescribed when over-the-counter supports do not provide releif and surgery can also offer a more permanent solution in severe cases. The board-certified doctors in our practice would be able to select the most appropriate course of action in each case.
Surgical Treatment

Rarely does the physician use surgery to correct a foot that is congenitally flat, which typically does not cause pain. If the patient has a fallen arch that is painful, though, the foot and ankle physicians at Midwest Orthopaedics at Rush may perform surgery to reconstruct the tendon and "lift up" the fallen arch. This requires a combination of tendon re-routing procedures, ligament repairs, and bone cutting or fusion procedures.
Prevention
Flat feet or Fallen Arches cannot be prevented due to congenital of nature or from underlying disease process; however, painful symptoms and future pathology from Flat Feet or Fallen Arches may be prevented by the following. Continue to wear your orthotics for work and exercise to provide stability and maintain function of your feet. Footwear. Continue to wear supportive shoes to maximise the function of your orthotic and prevent excessive movement of the joints in your feet.
Arch Pain Causes Symptoms And Treatments
Plantar fasciitis is a common, painful foot condition. Patients, and sometimes doctors often confuse the terms plantar fasciitis and heel spurs. Plantar fasciitis refers to the syndrome of inflammation of the band of tissue that runs from the heel along the arch of the foot; a heel spur is a hook of bone that can form on the heel bone (calcaneus). About 70% of patients with plantar fasciitis have been noted to have a heel spur that can be seen on x-ray.

Causes
Often, tarsal tunnel syndrome is misdiagnosed and confused with plantar fasciitis. Tarsal tunnel syndrome is when the tibial nerve which runs through the ankle, is pinched as it passes through the flexor retinaculum, the supportive band that surrounds the ankle joint. The symptoms of tarsal tunnel syndrome are often limited to the ankle but the since the nerve passes through the entire foot it can cause arch pain. Arch pain associated with foot strain is mainly caused by a pronated foot (rolls inward) or a flat foot. These are usually not singular causes of arch pain, but in combination with other factors, arch pain may result.
Symptoms
Intense heel pain, especially first thing in the morning and after a long day. Difficulty walking or standing for long periods without pain. Generally, the sharp pain associated with plantar fasciitis is localized to the heel, but it can spread forward along the arch of the foot and back into the Achilles tendon. While severe cases can result in chronic pain that lasts all day, the most common flare ups occur first thing in the morning, making those first steps out of bed a form of torture, and in the evening after having spent a day on your feet. Overpronation (a foot that naturally turns too far inward), high arches, and flat feet (fallen arches) can all cause similar arch pain. In these cases, however, the pain is more likely to continue throughout the day rather than being worst in the morning.
Diagnosis
The adult acquired flatfoot, secondary to posterior tibial tendon dysfunction, is diagnosed in a number of ways with no single test proven to be totally reliable. The most accurate diagnosis is made by a skilled clinician utilizing observation and hands on evaluation of the foot and ankle. Observation of the foot in a walking examination is most reliable. The affected foot appears more pronated and deformed compared to the unaffected foot. Muscle testing will show a strength deficit. An easy test to perform in the office is the single foot raise.
Non Surgical Treatment
Stretch the fascia. Prop your toes up against a wall, keeping your arch and heel flat so the toes stretch. Hold for a count of 10. Repeat 10 times three or four times per day. Roll a frozen water bottle under the arch. Stretch first then roll out the arch for 10 minutes; you don?t want to stretch the tendon when it?s ice cold. Freeze a golf ball and massage the fascia. Roll the frozen golf ball under the foot, starting from the front and working your way back. Put good pressure on each spot-the medial, center and lateral positions-for 15 seconds before moving to the next area. Then, roll the ball back and forth over the entire foot. Foam roll all muscles on the body above the plantar. Even tight shoulders can cause the condition, as your arm swing can throw off proper hip alignment and footstrike. Bump your arch. Get a commercial insole with an arch bump to push on the plantar and keep it from flexing-it doesn?t matter if you?re an under or overpronator; the plantar needs to be supported and strengthened, Wear the support in all shoes, if possible.

Surgical Treatment
As with most surgeries, patients and physicians should consider the surgery only after other, less invasive treatments have proven unproductive. Indications for surgery include Pain. Inability to function. Failure to improve after a six-month course of specific, directed physical therapy. Failure to improve after using arch supports, orthotics, or ankle and foot bracing. Once patients are at that point, the good news is that the procedure has considerably better outcomes than more traditional flat foot surgery. In the past, surgeons would realign and fuse the three hind joints, which would cause patients to lose motion, leaving them with a significantly stiff hind foot, With these newer procedures, if the foot is still flexible, surgeons can realign it and usually restore a close-to-normal or functional range of motion in the joints.
Prevention
There are several things you can do to prevent pain on the bottom of the foot. Here are some tips to help you avoid this condition. Do simple stretches each day (See Plantar Fasciitis Exercises for a list of all exercises). Wear good shoes that fit properly and are appropriate for the activity you are participating in. Lose excess weight if possible. Build your stamina slowly, especially with new exercises. Rest and elevate your feet, whenever possible, keeping them at least twelve inches above your heart. Always follow your doctor?s instructions for treatment. Each day do a different activity. For example: one day ride your bike, and swim the next day.